The role of haemoglobin and red blood cells in the transport of oxygen
The haematocrit test
to check the volume of cells in a blood sample
 Blood is drawn into a capillary tube, then one end is sealed and it is centrifuged to show the relative amounts of blood cells and fluid (plasma)
Blood is drawn into a capillary tube, then one end is sealed and it is centrifuged to show the relative amounts of blood cells and fluid (plasma)
Red blood cells occupy just under half the volume of the blood (about 45% for males, and 40% for females).
Haemoglobin inside the cells carries 98% of the oxygen in the blood, with the remaining 2% dissolved in water inside the cells and plasma outside them.
Red blood cells (erythrocytes) contain a large number of haemoglobin molecules, and practically none of the usual components of an ordinary body cell. There is no nucleus, and no mitochondria, endoplasmic reticulum, ribosomes, Golgi body.
Lacking a nucleus means that red blood cells are unable to perform which process?
>
cell division/mitosis
What is the consequence of that?
>
More cells must be produced permanently in bone marrow
Lacking mitochondria means that red blood cells are unable to perform which process?
>
AEROBIC respiration
What is the consequence (advantage?) of that?
>
Oxygen is not taken away (for use as electron acceptor)
Red blood cells clearly showing their biconcave disc shape
 Credit: Annie Cavanagh
Credit: Annie Cavanagh
The basically circular shape of red blood cells enables them to pass easily down blood vessels which are mostly cylindrical, and the narrowing in the centre allows red cells to fold over in the narrowest blood vessels - capillaries.
They also present a little more surface area (for gas exchange through the cell membrane) than they would if they were fatter, and their shape also enables them to withstand minor variations in the water potential of their surrounding fluid - blood plasma.
Inside the lungs, the circulation, the tissues
Within the lungs, oxygen gas from the air breathed in dissolves in the film of liquid lining the alveoli, and in its aqueous form it diffuses across the epithelium lining the alveoli then through the capillary wall and into the blood plasma. Next it enters the red blood cells and reacts with haemoglobin.
oxygen + haemoglobin → oxyhaemoglobin
This equation is in fact a slight over-simplification!
Blood leaving the lungs is oxygenated and the oxyhaemoglobin is transported inside the red blood cells all round the body.
In the tissues, oxyhaemoglobin breaks down, releasing oxygen.
oxyhaemoglobin → oxygen + haemoglobin
Another slight over-simplification!
Oxygen diffuses out of the red blood cells and into the blood plasma of the capillary bed where it passes by diffusion via tissue fluid into the respiring cells.
Erythropoiesis
This is the name given to the production of red blood cells:
erythrocytes. It is carried out under the influence of the hormone
erythropoietin, produced in the kidneys, in response to falling oxygen levels in the circulation.
Cells within the bone marrow regularly undergo cell division involving mitosis and the resulting cells go through a series of changes or 'differentiations'.
Each stage has a characteristic appearance and is given a different name. Some of these cells are quite large, and with a prominent nucleus.
The final stage, after removal of the nucleus, is called a
reticulocyte. Surprisingly it is still able to carry out protein synthesis and accumulate haemoglobin in the cytoplasm.
Finally, cell organelles (ER, Golgi, mitochondria) become bound up within vacuoles, subject to autophagy and removed by exocytosis.
It may be that this blebbing/shedding process results in the distinctive size and shape of the resulting erythrocyte.
Some statistics
Each human red blood cell contains approximately 270 million haemoglobin molecules.
The oxygen content (by volume) of oxygenated (arterial) blood is 20.4 ml/100 ml.
For comparison, the dissolved oxygen content of fresh water at blood temperature is 5.5 ml/L. This shows that haemoglobin in blood cells carries 37 times as much oxygen as can be carried by (fresh) water. The oxygen-carrying capacity of a solution isosmotic with body cell would be even lower.
Adult humans have roughly 20–30 trillion (2-3 × 10
13) red blood cells in the body.
The average adult has 4.5 to 5.5 litres of blood.
Women have about 4–5 million red blood cells per microlitre (cubic millimetre) of blood and men about 5–6 million.
The rate of red blood cell formation averages 2.4 million per second - 200,000,000,000 per day, (and also 10,000,000,000 white cells and 400,000,000,000 platelets per day).
Each (lap of the) circulation takes about 60 seconds (one minute).
The average life of a normal human red cell is 120 +/- 20 days.
The HbA1c test - nothing to do with oxygen transport
Haemoglobin reacts with glucose, and becomes 'glycated'. This can therefore be used to give an estimate of the body's exposure to elevated glucose concentrations over the last 2-3 months. This is especially important with type 2 diabetes.
A blood sample is sent to a laboratory where the level of glycation can be measured, usually using high-performance liquid chromatography.
Pulse oximetry
This is a simple procedure to measure the percentage saturation of oxygen in circulating blood, which ought to be quite high- 95-100%..
It could be used for people with a lung condition that affects their blood oxygen level, or to check that the body is functioning properly whilst an operation is being carried out (under anaesthesia).
A small device is clipped onto the finger or earlobe. This emits and detects light at two wavelengths.
Oxygenated blood absorbs infrared light and lets ordinary red light through, whereas deoxygenated blood does the reverse.
In hospitals this can easily be connected to a monitoring station displaying the percentage saturation, and setting off an alarm if the value falls.
Alternatively small display units can be used when investigating the effects of exercise on the body.



 Blood is drawn into a capillary tube, then one end is sealed and it is centrifuged to show the relative amounts of blood cells and fluid (plasma)
Blood is drawn into a capillary tube, then one end is sealed and it is centrifuged to show the relative amounts of blood cells and fluid (plasma)
 Credit: Annie Cavanagh
Credit: Annie Cavanagh





 No actual values for partial pressure, but I have added a reference point for the condition in the placenta
No actual values for partial pressure, but I have added a reference point for the condition in the placenta

 Altitude:4335m
Altitude:4335m
 Here we see a sheep grazing on Mount Snowdon: altitude about 1000m
Here we see a sheep grazing on Mount Snowdon: altitude about 1000m



 Nobody has bothered to put any numbers on the x-axis but I think the p50 is about level with the 'i' in partial. And of course 0.2 kPa must be level with the 'u' in pressure.
Nobody has bothered to put any numbers on the x-axis but I think the p50 is about level with the 'i' in partial. And of course 0.2 kPa must be level with the 'u' in pressure.

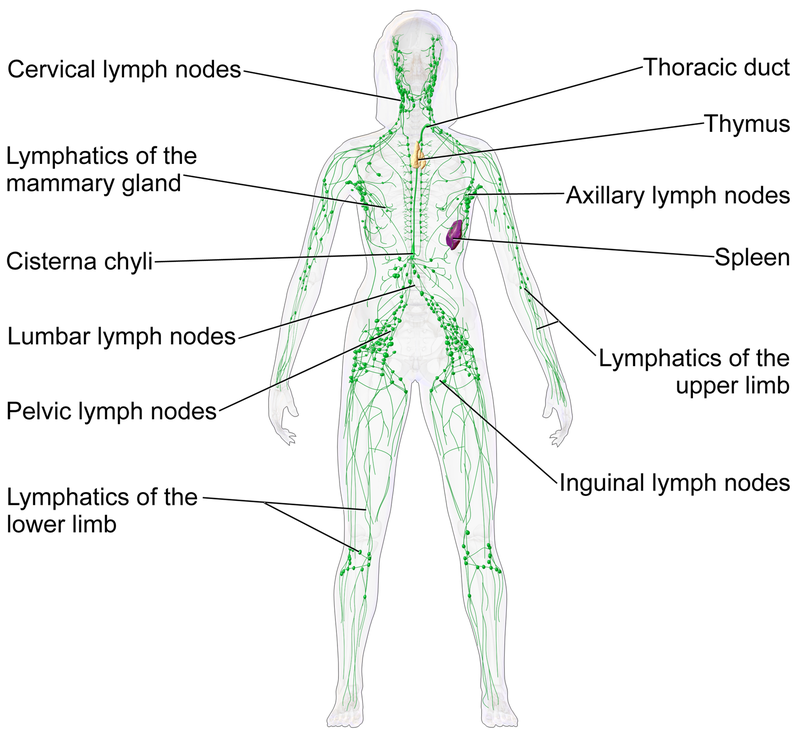
 This is a simplified diagram. It does not show left and right organs, and the body is not rectangular.
This is a simplified diagram. It does not show left and right organs, and the body is not rectangular.
 This somewhat stylised diagram shows blood vessels containing oxygenated blood in red, and blood vessels containing deoxygenated blood in blue.
This somewhat stylised diagram shows blood vessels containing oxygenated blood in red, and blood vessels containing deoxygenated blood in blue.

 The right coronary artery is the first artery to branch off the aorta, and the circumflex artery is a branch of the left coronary artery. These supply oxygenated blood to the (outside of) the heart muscle, and the associated veins return deoxygenated blood to the vena cava.
The right coronary artery is the first artery to branch off the aorta, and the circumflex artery is a branch of the left coronary artery. These supply oxygenated blood to the (outside of) the heart muscle, and the associated veins return deoxygenated blood to the vena cava.

 Blood pressure is taken using a pressurised cuff round the arm.
Here the pressure at which blood flow stops and starts is monitored using a stethoscope.
Blood pressure is taken using a pressurised cuff round the arm.
Here the pressure at which blood flow stops and starts is monitored using a stethoscope.


 Source:
Source:




 Medical gallery of Blausen Medical 2014
Medical gallery of Blausen Medical 2014

